January 27, 2025
Ocular Melanoma
A look into the second most common melanoma diagnosis.
Understanding Ocular Melanoma.
Many questions can arise when talking about ocular melanoma: How do I prevent it? How is it diagnosed? What do I need to know to keep me and my family safe? Our team has assembled the sections below to help you navigate your or your loved one’s ocular melanoma journey.

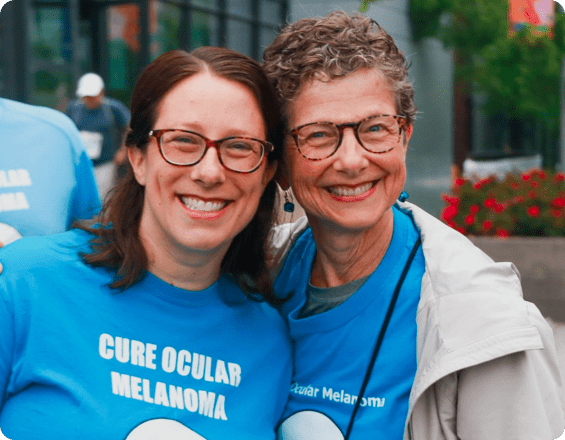
About the MRF’s CURE OM Initiative.
CURE OM (the Community United for Research and Education of Ocular Melanoma) is the MRF’s initiative to increase awareness, education and research funding for ocular melanoma, while improving the lives of people affected by this disease. Founded in 2011, the CURE OM initiative excels because of the hard work and dedication of its Patient and Scientific Steering Committees and the generosity of our community. Show your support with a tax-deductible donation to the CURE OM initiative today!
About Ocular Melanoma.
Ocular melanoma (OM) is a form of melanoma that develops in the eye and is the most common primary intraocular (inside the eye) cancer in adults. There are nearly 2,000 – 2,500 new cases diagnosed each year in the United States, and it is the second most common type of melanoma (after cutaneous (skin) melanoma).¹
Like other melanomas, it grows from melanocytes – the cells that produce the pigment melanin that colors the skin, hair, and eyes, and can form moles on the skin. In the eye, melanocytes are found in the uvea (iris, ciliary body, and choroid), which is where ocular melanoma most often develops. It is also known as uveal melanoma when found in the uvea but commonly referred to as ocular melanoma.
If you have ocular melanoma, it is important to know your diagnosis, and treatment options.
We have provided resources for people diagnosed with OM. About one quarter of all OM cases spread (metastasize) to other parts of the body, most commonly the liver. When this occurs, it is more difficult to treat than cutaneous melanoma but new treatments are emerging. More information about this type of melanoma is available in our OM Fact Sheet.


Types of Ocular Melanoma
Different types of melanoma of the eye include:
Uveal Melanoma
Melanoma that arises in the uvea, the middle layer of the eye, which includes the choroid, iris, and ciliary body. Uveal melanoma can form in any of these layers and is named for where it forms:
- Choroidal melanoma begins in the layer of blood vessels – the choroid – beneath the retina. It is the most common type of uveal melanoma. Choroidal nevi (benign pigmented spots) can sometimes transform into choroidal melanoma, so regular monitoring by an ophthalmologist is important.
- Iris melanoma occurs in the front, colored part of the eye. Iris melanomas usually grow slowly and less commonly spread (metastasize) to other parts of the body.
- Ciliary melanoma occurs in the part of the eye between the iris and the choroid. Tumors in the ciliary body are more likely to grow larger before being detected and may have a higher risk of metastasis.
Conjunctivial Melanoma
The conjunctiva is the clear tissue that covers the white part of the eye, as well as the inside of the eyelids. Conjunctival melanoma is an extremely rare form of eye melanoma. It often appears as a raised tumor and may contain little or even no pigment. Conjunctival melanoma most commonly occurs in the bulbar conjunctiva, the membrane that covers the outer surface of the eyeball.
Unlike uveal melanoma, which most often spreads to the liver, conjunctival melanoma is more likely to spread (metastasize) to regional lymph nodes and the lungs.
Frequency, Incidence & Risk Factors of Ocular Melanoma
About 5-6 people per million are diagnosed with ocular (uveal) melanoma in the US each year. In comparison, invasive melanoma of the skin occurs in approximately 1 in 38 Americans over a lifetime. The incidence of ocular melanoma is similar in other populations of European ancestry. Ocular melanoma accounts for about 3-5% of all melanomas.
While the incidence of cutaneous (skin) melanoma has increased over the last several decades, ocular melanoma rates have remained relatively stable.
A variety of risk factors have been identified for ocular melanoma, including light-colored eyes, fair skin, dysplastic nevus syndrome and mutations in the BAP1 gene. The role of sun exposure as a risk factor for ocular melanoma remains unclear.
Ocular Melanoma tends to occur slightly more often in males than in females and overall risk tends to increase with age.
Early detection is critical. Because many people do not notice symptoms, ocular melanoma is often found during a routine dilated eye exam. Detecting OM early gives patients more treatment options and can help preserve vision and improve outcomes.
#EYEGETDILATED
OM Patient & Caregiver Resources
Education
The CURE OM (Community United for Research and Education of Ocular Melanoma) initiative is committed to being the leading provider of ocular melanoma education, resources and support. We partner with OM clinicians and researchers to ensure our OM patient and caregiver community receives the most up-to-date and accurate information.
Through the #EyeGetDilated campaign, CURE OM aims to increase awareness by promoting the importance of early detection. OM is most often detected during a routine, dilated eye exam.
Eyes on a CURE: Patient & CaregiverSymposium – CURE OM hosts an annual educational symposium in collaboration with major academic medical centers. These meetings provide opportunities to learn from leaders in ocular melanoma and to connect with other OM patients and caregivers. Experts provide updates on diagnosis, treatment options, clinical trials and research. View past Symposium recordings and learn about upcoming meetings here:

Find Support
CURE OM offers virtual support groups to individuals diagnosed with primary and metastatic ocular melanoma (OM). These virtual sessions provide a mix of educational and wellness information, as well as space to connect with other patients for emotional support and companionship. We ask that these groups remain a safe space – free of judgment or any direct medical advice. For more information about participating in a virtual OM support group please email us at cureom@melanoma.org ror more information and to register.
Find an OM Specialist.
Use the Treatment Center Finder to explore ocular melanoma treatment centers. Please note, this is not a doctor’s recommendation list, simply a list of OM specialists to get you started. The Eye Cancer Network also provides a list of specialists in the US and more than 50 countries around the world.

Form a CURE OM Miles for Melanoma Team
Miles For MelanomaAttend a Gala
Galas & Signature EventsStart a CommUNITY Fundraiser
CommUNITY FundraisingVISION Registry Discussions Boards
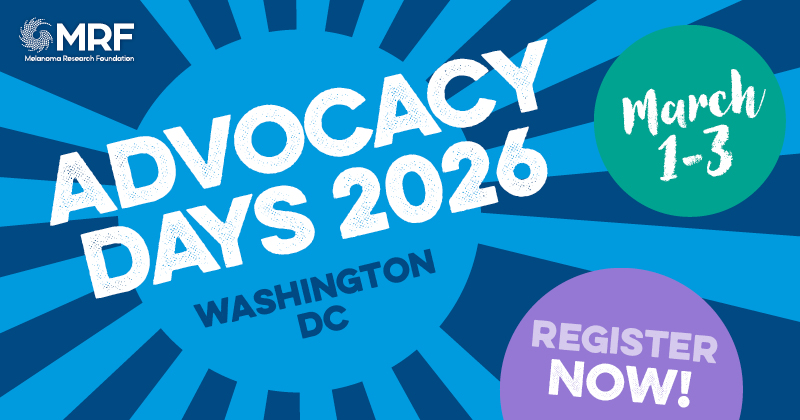
VISION RegistryAdvocate at State & Federal Level
Advocate for MelanomaOM Research
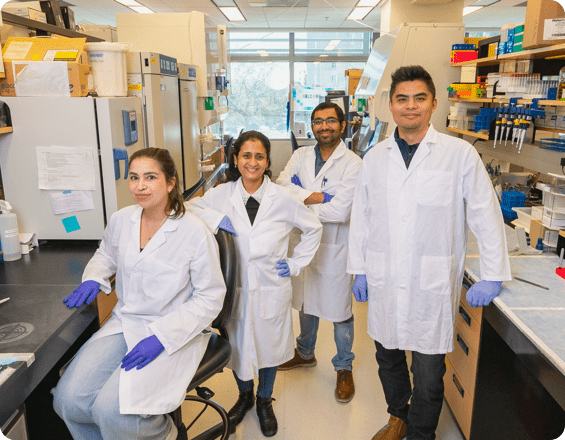
The CURE OM initiative is leading the ocular melanoma (OM) field forward. We are committed to accelerating the development of effective treatments and, ultimately, a cure for this disease. Our scientific initiative includes research grants, a patient registry and biannual international scientific meetings. These efforts ensure continued collaboration, support and coordination to move OM research forward.
To date, the MRF has funded over 24 uveal melanoma grants totaling over $2.6 million. To learn about upcoming CURE OM research opportunities, visit our Research Grants RFP Page. To learn more about past uveal melanoma research grantees, visit our Funded Research Page and filter by melanoma type → Ocular Melanoma.
Researchers/Clinicians: to learn more about the CURE OM research opportunities, please contact CUREOM@Melanoma.org.
CURE OM hosts regular global science meetings to facilitate interdisciplinary and innovative collaboration focused on finding effective treatments and, ultimately, a cure for ocular melanoma. Each meeting includes a diverse group of speakers and participants from around the world. To learn more about upcoming & past CURE OM scientific meetings, search our Scientific Meetings Page.

Vision Platform
In 2021, CURE OM launched the VISION Registry, a global patient-reported registry to support advances in ocular melanoma research and treatment development. Designed with the guidance of the Registry Steering Committee, the VISION Registry will inform patient-centered research initiatives focused on policy, patient preferences and standards of care. In addition to collecting invaluable data about diagnosis, disease progression, treatment choice and outcomes, geography and environmental factors, the registry supports the collaboration of patients, caregivers, clinicians, researchers, and the pharmaceutical industry to find a cure together.
In 2023, the MRF’s CURE OM initiative expanded the VISION Registry to create the VISION Platform. The goal of the VISION Platform, is to unite the global ocular melanoma (OM) community by providing an interactive and innovative central place where dispersed patients and caregivers can access disease-specific resources and tools and share their knowledge and experiences with each other and to advance research. The VISION Platform continues to grow in collaboration with OM patient and community input and feedback and currently encompasses the following key components:
Thank you for your interest in VISION.
The VISION Platform is on a temporary administrative hold. If you are already enrolled in VISION you will be notified by email when the study is up and running again. If you are not already enrolled and/or have questions or concerns or require additional resources please reach out to Miriam Kadosh at mkadosh@melanoma.org. Thank you for your patience!
Clinical Trials
The CURE OM Clinical Trial Finder will help you understand which emerging ocular melanoma treatments may be an option for you. Clinical trials offer OM patients the opportunity to receive care that may not yet be standard. You must be logged in via the VISION Registry to access the OM Clinical Trial Finder.
Looking for treatment options or want to learn more about what’s available in ocular melanoma treatment? The Melanoma Research Foundation’s Clinical Trials Finder is a free, easy-to-use tool that helps patients and caregivers explore clinical trials that may be a match. To get started, click here.
Citations
Content last updated: August 26, 2020
Cheung A, et al. Distinguishing a Choroidal Nevus From a Choroidal Melanoma. American Academy of Ophthalmology. 2012. Accessed August 26, 2020.
Krantz BA, Dave N, Komatsubara KM, Marr BP, Carvajal RD. Uveal melanoma: epidemiology, etiology, and treatment of primary disease. Clin Ophthalmol. 2017;11:279-289. Published 2017 Jan 31. doi:10.2147/OPTH.S89591
Meeting Report From the 2023 Cure Ocular Melanoma (CURE OM) Global Science Meeting, Philadelphia, PA, November 2023 – PubMed. Seedor, R. S., Aplin, A. E., Bertolotto, C., Carvajal, R. D., Deacon, N., Doble, K., … Selig, S. M. (2025). Meeting report from the 2023 Cure Ocular Melanoma (CURE OM) Global Science Meeting, Philadelphia, PA, November 2023. Pigment Cell & Melanoma Research, 38(1), e13205.
https://link.springer.com/article/10.1007/s11912-025-01684-0?utm_source=chatgpt.com. Dhar, A., Choudhary, A., & Kaliki, S. (2025). State-of-the-art in metastatic uveal melanoma treatment: A 2025 update. Current Oncology Reports, 27(5), 199–214. Expert reviewers: Dr. Ivana Kim and Dr. Shaheer Khan.