
Jon Ziska’s Melanoma Story
Guest blog post by Jon Ziska, melanoma thriver and advocate: “My Melanoma Journey began with a “normal wellness check” AKA annual physical. I was in the d...
Learn more about our upcoming Galas and Signature Events Learn More

Guest blog post by Ian Michael Crumm, Celebrity Esthetician, Podcast Host, Key Opinion Leader, Melanoma Advocate and 2025 #GetNaked Spokesperson: Some moments stick with yo...

Guest blog post by Jon Ziska, melanoma thriver and advocate: “My Melanoma Journey began with a “normal wellness check” AKA annual physical. I was in the d...

Cleveland, OH (July 10, 2025) – The Melanoma Research Foundation (MRF) is thrilled to announce one of the next events in its annual Miles for Melanoma nationwide 5K p...

“Leveraging T Cell Genetic Variants to Enhance Melanoma Immunotherapies” T cell immunotherapies, which harness the power of a patient’s own immune system to t...

“Dad loved spending time with his family. He cherished being together, from spontaneous dinner gatherings to afternoon visits, to holidays and birthday celebrations. He w...

The Melanoma Research Foundation Launches its Annual Chicago 5K Fundraiser with a Goal of $100,000 in Support of its Mission Chicago, IL (June 25, 2025) – The M...

Guest blog post by Melissa Kultgen, Melanoma Survivor and Advocate: As a cheerleader, Melissa Kultgen grew up in “toxic tan culture” and was bullied for having such pal...

I was diagnosed with Melanoma in February 2025. Here is my story … I have always been a lover of the sun … and said I am solar powered several times. I grew u...

The 2025 American Society of Clinical Oncology (ASCO) Annual Meeting was held from May 30 to June 3. This world’s largest clinical cancer research conference brought toge...

The 2025 American Society of Clinical Oncology (ASCO) Annual Meeting was held from May 30 to June 3. This world’s largest clinical cancer research conference brought toge...

Denver, CO (May 27, 2025) – The Melanoma Research Foundation (MRF) is thrilled to announce the next event in its annual Miles for Melanoma nationwide 5K program, brin...

Hi, I’m Amy Nichole, a portrait and landscape photographer, content creator for our travel page Adventure Our Life, and proud dog mom to my sweet girl, Roxy. While I’m ...

Guest blog post by Kora Kane, Melanoma Patient: I was 23, just a year out of college. My biggest goals consisted of very early twenties ideas: to buy an apartment and...
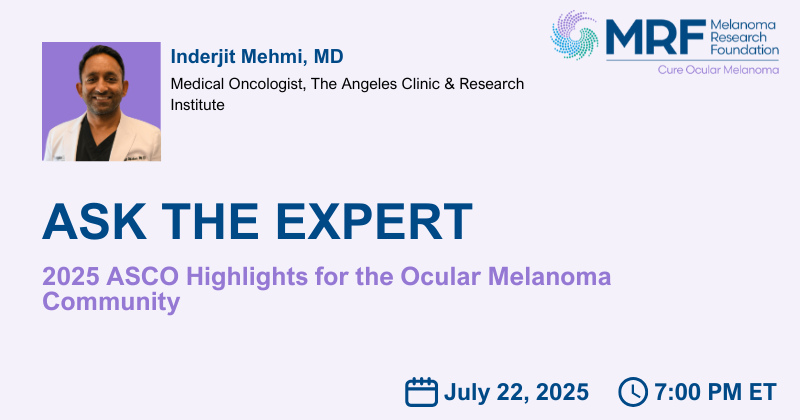
Jul 22, 2025 ET




