January 27, 2025
Prevention & Awareness
Can Melanoma Be Prevented?
Nearly 93% of cutaneous melanoma cases in the US are attributable to ultraviolet (UV) exposure. This is a major risk factor that you can prevent over the course of your lifetime. The MRF is committed to increasing awareness of melanoma prevention and early detection.

Melanoma Prevention
It’s best approached in two ways.

Primary Prevention
Defined as reducing or limiting exposure to UV radiation to prevent melanoma from occurring.

Secondary Prevention
Defined as detecting melanoma in its earliest stages through regular screenings.
Prevention
These tips can help protect you:
Seek shade when possible
Between the hours of 10 am – 2pm, UV light is the strongest and your chance of skin cancer and skin aging increases significantly.
It’s important to either seek shade or avoid staying outside for longer periods during these times. Checking the UV index every morning on your phone is also an easy way to gauge when it’s safe to be outside. Anything above level 2 warrants caution!
Cover up
Broad spectrum sunscreen (SPF 30+) application all over your body and sun protective clothing should be worn year-round regardless of:
- The weather – 80% of the sun’s harmful UV rays can penetrate your skin on cloudy days. Waters, snow, and sand reflect and magnify the damaging rays of the sun, increasing your chance of sunburn.
- Perceived skin cancer risk – everyone is at risk for melanoma despite age, skin color, gender identity, or family history.
Each time you apply sunscreen, use about one ounce (a shot-glassful) and apply 15 minutes before sun exposure — reapply every two hours and immediately after swimming or sweating. Be sure to also cover up with long sleeved pants and shirts, wide brimmed hats, and sunglasses. See below for more information.
Avoid Tanning and Sunburns Entirely
There is no such thing as a safe or healthy tan. Just ONE indoor tanning session increases your chance of skin cancer by 75%. Skin damage is cumulative, for every tan, risk of melanoma increases substantially.
Monthly Self Skin Exam
YOU are most likely to first spot melanoma on your skin. Routinely examine your skin and any moles to identify any changes early on. Put your selfie skills to good use and photograph your moles or use a mole mapping app to keep track of any changes in your skin. If you do notice any changes in your skin or moles, prioritize seeing your primary care provider or dermatologist immediately.
Use the ABCDE’s of Melanoma to know what to look out for and help monitor any changes. A mirror can help check areas that are hard to see, such as your shoulders, back, and groin area. The Self Screening Guide for the how-tos of self-skin exams.

Youth Prevention
Learn more about sun safety for babies, infants and school-age children!
Learn MoreEarly Detection
Teens and young adults can enjoy life and still practice sun safety habits!
Learn MoreFacts About Cutaneous Melanoma Prevention
- Nearly 93% of melanomas are thought to be caused by exposure to UV light and sunlight.
- It takes only one blistering sunburn, especially at a young age, to more than double a person’s chance of developing melanoma later in life.
- Indoor tanning beds are proven to cause cancer and have been classified into the highest cancer risk category by the World Health Organization’s International Agency for Cancer Research (IARC).
- Young people who regularly use tanning beds are 8 times more likely to develop melanoma than people who have never used them.
However, some risk factors for cutaneous melanoma cannot be prevented:
Look Out For:
Visit the American Cancer Society for additional details about the condition and its relationship with cutaneous melanoma.2
Additionally, some risk factors for ocular melanoma also cannot be prevented:
Look Out For:
Visit the National Comprehensive Cancer Network’s Uveal Melanoma Guidelines for additional details about the condition and its relationship with ocular melanoma.2
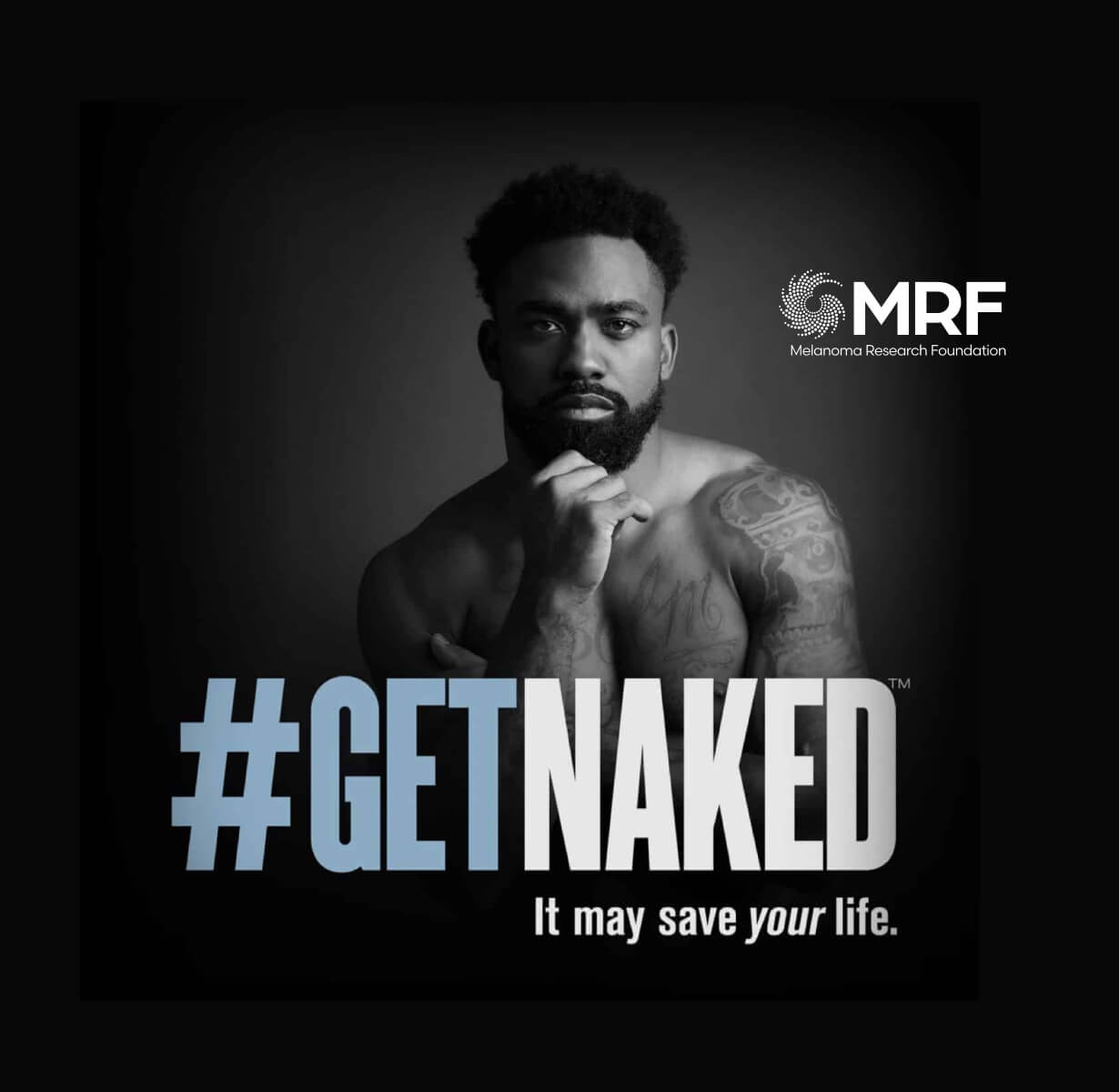
Awareness Campaigns
Approximately 90% of melanomas are considered preventable.
The MRF is committed to increasing awareness of melanoma prevention and early detection while offering the most helpful resources for treatment, survivorship and support. Learn more about our current awareness campaigns and the inspiring individuals they highlight.
Additional Prevention Resources:
Cutaneous Melanoma Prevention
Citations
Content last updated July 2024
Proportion and number of cancer cases and deaths attributable to potentially modifiable risk factors in the United States, 2019. CA: A Cancer Journal for Clinicians, 2024 Jul 11. doi: 10.3322/caac.21858.
American Cancer Society, https://www.cancer.org/cancer/melanoma-skin-cancer/causes-risks-prevention/risk-factors.html
National Comprehensive Cancer Network: Uveal Melanoma Guidelines, https://www.nccn.org/professionals/physician_gls/pdf/uveal.pdf
Suppa M, Daxhelet M, del Marmol V. Dépistage du mélanome [Melanoma secondary prevention]. Rev Med Brux. 2015;36(4):255-259.



