January 27, 2025
Early Detection
The more you mela-KNOW-ma may save your life!
Early Detection
Cutaneous Melanoma
You are most likely to first spot a melanoma on your skin. It’s important to know your skin and its moles and other characteristics so it’s easier to identify any changes early. Knowing the ABCDEs and how to conduct your own skin exam may be lifesaving. Check out the More You Mela-KNOW-ma guide to learn more about what to look for when performing a self-skin exam.

Early Detection for Rare Melanoma Subtypes
Acral Melanoma
Acral : Acral lentiginous melanoma (ALM) is the most common melanoma found in people of color, often appears in hard-to-spot places, including under the fingernails or toenails, on the palms of the hands or soles of the feet. Website found: Melanoma Warning Signs and Images – The Skin Cancer Foundation
Things to look for:
- Sore that won’t heal or heals and then returns.
- Sore that has a hard time healing. Pay special attention if the sore appears in a scar or on skin that was previously injured.
- Patch or spot on skin that feels rough and dry.
- Dark line or spot underneath or around a fingernail, toenail, or palms of hands and feet.
- Dark spot, growth, or darker patch of skin that is growing, bleeding or changing in any way.

Early Detection for Rare Melanoma Subtypes
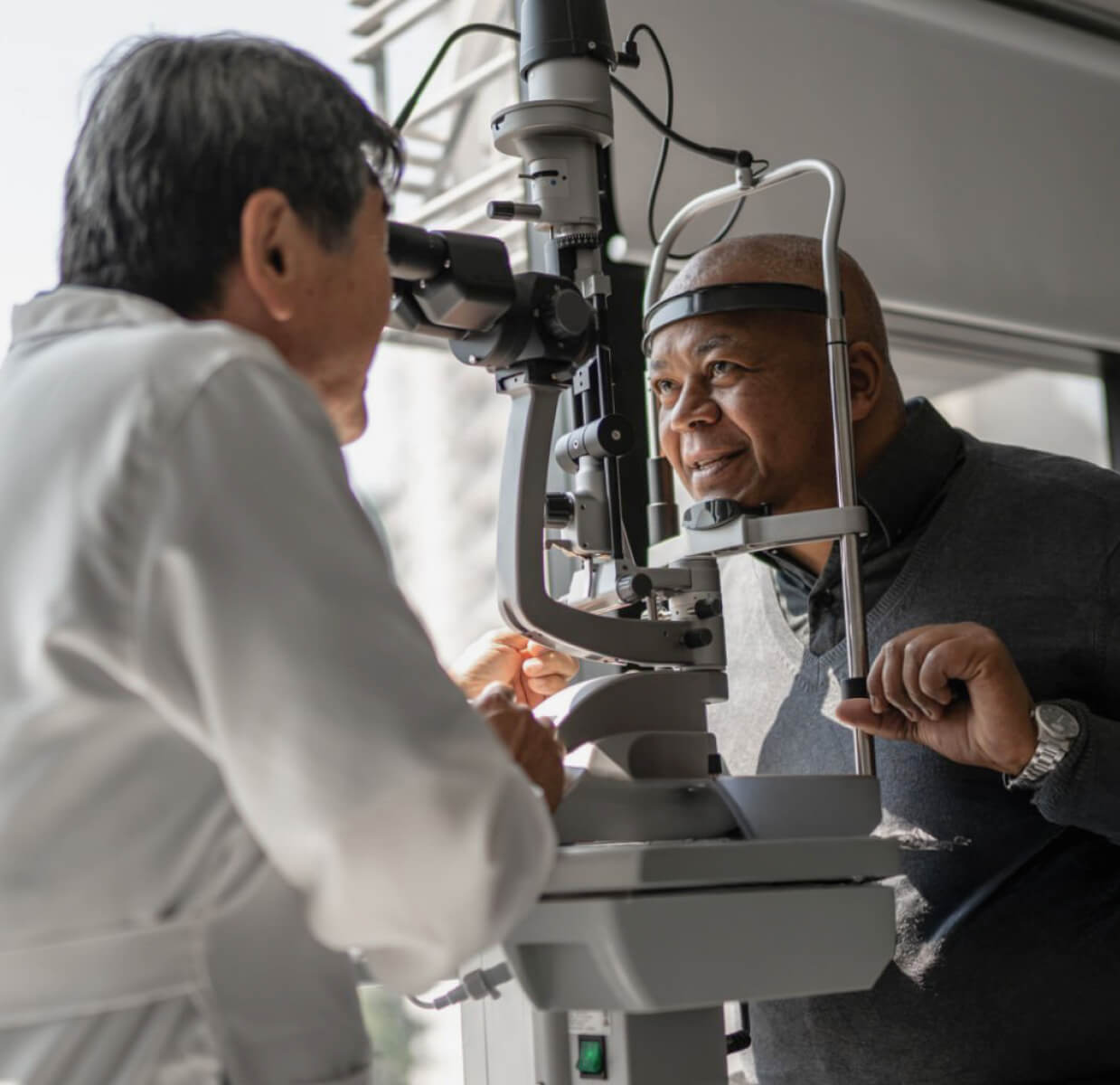
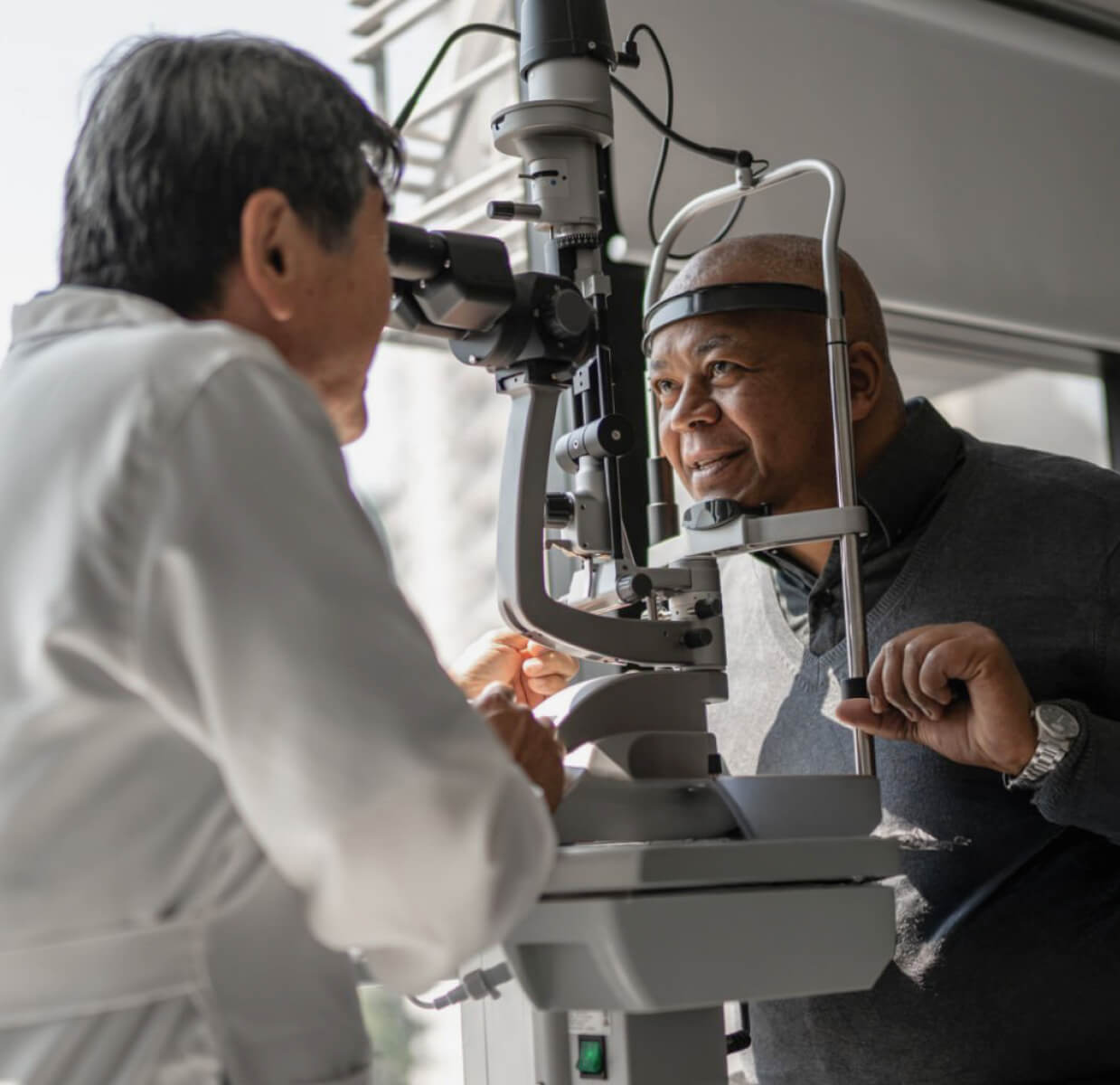
Ocular Melanoma
Ocular melanoma (OM) is an aggressive form of melanoma affecting the structures of the eye. OM is detected during a routine eye exam and therefore, visiting your optometrist or ophthalmologist regularly is critical. (From our website and from this site: American Cancer Society, https://www.cancer.org/cancer/eye-cancer/causes-risks-prevention/prevention.html)
Ocular melanoma (OM) is an aggressive form of melanoma and is the most common form of eye cancer in adults. It is diagnosed in approximately 2,000 Americans each year. There are no specific PREVENTION recommendations, but limiting UV exposure by wearing sunglasses may be helpful.⁶
OM is often detected during a routine eye exam, so scheduling your yearly exam that includes a dilated eye exam as recommended by the American Academy of Ophthalmology is the best form of EARLY DETECTION.⁷

Report any eye changes:
Development of a dark spot (or a “freckle”) on your eye
Vision changes such as blurriness or a blind spot
The sensation of flashing lights
Change in pupil shape
Early Detection for Ocular Melanoma
Diagnosing OM at an early stage is important for a better outcome.
Ocular melanoma (OM) is a form of melanoma that develops in the eye and is the most common primary eye tumor in adults. There are nearly 2,000 new cases diagnosed each year in the United States, and it is the second most common melanoma (after cutaneous melanoma).¹ Like other melanomas, it begins as melanocytes – the cells that produce the pigment melanin that colors the skin, hair, and eyes, as well as forms moles. If you have ocular melanoma, it is important to know your diagnosis, and treatment options. We have provided resources for people diagnosed with OM. Fifty percent of these cases spread to other parts of the body. When this occurs, it is most often fatal. More information about this type of melanoma is available in our OM Fact Sheet.

Early Detection for Ocular Melanoma
How is Ocular Melanoma Diagnosed?
Ocular melanoma (OM) is most often detected by an optometrist or an ophthalmologist during a dilated eye exam. Often, OM is asymptomatic until the tumor grows large enough to create visual disturbances. Only OM of the iris can be diagnosed by external – from the outside – examination.
After an OM diagnosis, your doctor may want to take an X-ray, MRI or CT scan of the body to check the body for signs of cancer beyond the eye.
Unlike other forms of melanoma, a biopsy is not usually taken to diagnose OM. Rather, OM tends to be a clinical diagnosis – meaning it is often made based on signs and symptoms.
If you or a loved one have been diagnosed with OM, or to learn more about OM research, treatment and support resources, please visit the MRF’s CURE Ocular Melanoma (CURE OM) initiative.

Early Detection in Ocular Melanoma
Frequency, Incidence & Risk Factors of Ocular Melanoma:
6 people per 1 million are diagnosed with eye melanoma in the US every year, while invasive melanoma of the skin occurs in approximately 1 in 50 Americans each year. The incidence of ocular melanoma is similar in other Caucasian populations worldwide. According to a 2017 article published in Clinical Ophthalmology, melanoma of the eye accounts for approximately 3-5% of all melanomas². Melanoma of the skin increased in frequency over the last several decades, while such a trend is less evident with ocular melanoma.
A variety of risk factors have been identified for ocular melanoma, including light eyes, fair skin type, dysplastic nevus syndrome and the BAP1 mutation. The role of sun exposure as a risk factor for ocular melanoma remains unclear.
Melanoma of the eye tends to occur slightly more often in males than in females and overall risk tends to increase with age.

Early Detection for Mucosal Melanoma
Mucosal Melanoma
Mucosal melanoma often goes misdiagnosed, mostly because of the anatomical locations of the disease and because of the lack of discernible signs and symptoms. For instance, melanoma of the ano-rectal region is often misdiagnosed as hemorrhoids.
Signs & Symptoms of Mucosal Melanoma
- Mucosal melanoma symptoms vary greatly. If you notice any of these signs or symptoms, it’s important to let your doctor know right away:
- A suspicious spot in your mouth or nasal passages
- Unexplained sores or sores that won’t heal
- Unexplained bleeding from the rectum or vagina
- Hemorrhoids that won’t heal or seem to worsen
- Pain during a bowel movement
Have You Been Diagnosed with Mucosal Melanoma?
- First, know that you are not alone. Second, arm yourself with information on mucosal melanoma and learn about available mucosal melanoma treatment options.
- You may also find these Questions to Ask Your Doctor useful.
Early Detection for Rare Melanoma Subtypes
Mucosal Melanoma
Mucosal melanoma is a rare form of melanoma that occurs in the mucosal surfaces of the body such as the sinuses, nasal passages, oral cavity, vagina, vulva, anus and other areas. Unlike most cases of melanoma of the skin, mucosal melanoma is not considered to be related to or affected by UV exposure. Additionally, there are no obvious identified risk factors, not even family history, so PREVENTION strategies aren’t identified yet.⁹ Lacking an identifiable culprit and given its rare occurrence, most cases of mucosal melanoma are quite advanced once identified.
Mucosal melanoma is found in the in the mucosal areas of the body including the nasal passages, mouth, vagina, and anus and are not considered to be related to UV exposure. Routine visits with a variety of healthcare providers including:
- OBGYNs
- Dentists
- Ear, nose, and throat specialists (ENTs)
are the most important steps you can take for early detection of mucosal melanoma.
Early Detection for Rare Melanoma Subtypes
Pediatric Melanoma
A proper diagnosis is essential for selecting the best treatment. The diagnosis of skin melanoma can only be made with a biopsy, which is then examined under a microscope by a pathologist. Pathologists who specialize in looking at skin biopsies are called dermatopathologists, but even board-certified dermatopathologists may not have extensive expertise in recognizing melanoma in children. In addition, even expert dermatopathologists sometimes disagree about the classification of a child’s mole as benign, atypical or malignant. It is important to be sure that an expert dermatopathologist has looked at your child’s biopsy, and you especially need to know if there is some degree of uncertainty about whether the mole is benign, atypical or malignant. Sometimes, highly specialized diagnostic tests like FISH and CGH are used to better classify pediatric lesions.

Early Detection for Rare Melanoma Subtypes
Pediatric Melanoma
Because pediatric melanoma is difficult to diagnose, the diagnosis can sometimes be delayed or misdiagnosed. Most doctors don’t expect it, and some types of pediatric melanoma look different than adult melanoma. Sometimes pediatric melanoma is misdiagnosed as pyogenic granulomas, atypical melanocytic neoplasms, warts or spitz nevi.
If the biopsy comes back as a melanoma, surgeons may perform another surgery to ensure there are clear margins – the term used for the complete removal of the lesion. Depending on the diagnosis, the doctor may recommend a sentinel lymph node mapping, and depending on those results, a lymph node resection may be performed. This will help the doctors know if the melanoma has spread beyond the primary tumor. All of this information will be included in pathology report. The pathology report will help you understand your child’s stage of diagnosis, as well as help guide your treatment options.
Melanoma does not discriminate – NEVER LET A DOCTOR TELL YOU THAT YOUR CHILD IS TOO YOUNG TO GET MELANOMA.
Learn more about melanoma and how it is staged.

What does pediatric melanoma look like?
Your child’s skin should be evaluated by a professional familiar with pediatric melanoma if you see any area with one of the following features:
- A bump that itches and bleeds
- A spot that looks like an unusual wart – sometimes non-pigmented or with a pinkish color
- An amelanotic lesion – a lump on the skin that isn’t dark or black (like many adult melanomas)
- A mole that becomes nodular – very bumpy and sticking out far from the rest of the skin
- A lesion that presents as a nodule, or lump, especially one that has been rapidly enlarging
- Moles that look strange or large – especially a mole that looks DIFFERENT from your child’s other moles or has more than one color
Although some research suggests that the ABCDEs of melanoma should be revised when using them for diagnosing melanoma in children, it is important to remember that in most cases, the E, for evolution or change, is the most important factor to consider.
What if I spot something suspicious?
Screening for melanoma starts at home. Parents should be aware of all moles that their children have so that they will notice any changes or new moles.
A dermatologist, preferably one who has a lot of experience in melanoma, should examine your child’s skin immediately. Alternatively, you may wish to have your child examined at a pediatric pigmented lesions clinic or by a pediatric oncologist experienced in pediatric melanoma. It is important that melanoma is detected as early as possible to ensure the best outcome.
Check out our Kid’s Guide to Self-Screening!




