January 27, 2025
Melanoma Facts & Stats
Melanoma diagnoses are increasing at epidemic rates. You can help make a difference by knowing and sharing the facts about melanoma.
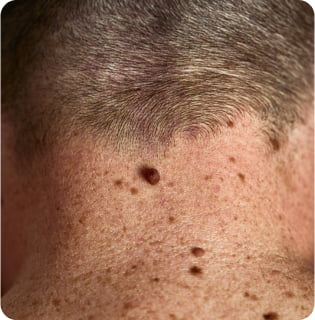
Melanoma Diagnosis Facts
- Melanoma is the deadliest form of skin cancer. Skin cancer is the most common form of cancer in the U.S.
- In 2023, nearly 187,000 Americans are expected to be diagnosed with melanoma. Of these, more than 97,600 will be diagnosed with invasive (Stage I, II, III or IV) melanoma and over 89,000 will be diagnosed with melanoma in situ (Stage 0).1
- In 2023, melanoma is expected to take the lives of 7,990 Americans.1
- Melanoma is not just skin cancer. It can develop anywhere on the body – eyes, scalp, nails, feet, mouth, etc.
- Melanoma does not discriminate by age, race or gender.
- In ages 30-39, melanoma is the fifth most commonly diagnosed form of cancer.
- The incidence of people under 30 developing melanoma is increasing faster than any other demographic group, soaring by 50% in women since 1980.
- Approximately 400 children in the U.S. are diagnosed with melanoma each year.
- Melanoma rates in the United States doubled from 1982 to 2011 and have continued to increase.5
- Today, approximately 1.3 million people live with melanoma in the U.S.4
- The lifetime risk of getting melanoma is about 1 in 40 for Caucasians, 1 in 200 for Hispanics and 1 in 1,000 for African Americans.
- People of color are more likely to get melanoma in areas that don’t see the sun – like the palms of the hands, the soles of the feet, under the nails.6
- Skin cancer in people of color is often diagnosed in later stages, making it more difficult to treat.6
- Ocular melanoma, or melanoma of the eye, is the most common primary eye tumor in adults with around 2,000 new cases diagnosed each year in the United States.7
- Mucosal melanoma is a rare form of melanoma that develops in the sinuses, nasal passages, oral cavity, vagina, anus and other areas, making up about 1% of melanoma cases.8
The MRF is proud to offer the Melanoma Fact Sheet in the following languages:
Melanoma Prevention Facts
- Nearly 90% of melanomas are thought to be caused by exposure to UV light and sunlight.9
- Experiencing five or more blistering sunburns between ages 15 and 20 increases one’s melanoma risk by 80 percent.10
- You can help prevent melanoma by seeking shade whenever possible, wearing protective clothing, avoiding direct sunlight between 10am-4pm and using broad spectrum sunscreen with SPF of at least 30 every day.
Indoor & Intentional Tanning Facts
- Indoor tanning devices are proven to cause cancer and have been classified into the highest cancer risk category by the World Health Organization’s International Agency for Cancer Research (IARC).11
- A comprehensive meta-analysis concluded that the risk of cutaneous melanoma is increased by 75% when use of tanning devices starts before 30 years of age.11
- Research has found that indoor tanning does not protect against sunburn.12
- Having 5 or more blistering sunburns early in life increases one’s melanoma risk by 80%.13
Citations
Content last updated: February 6, 2023
North American Association of Central Cancer Registries (NAACCR). Estimated deaths are based on 2003-2017 US mortality data, National Center for Health Statistics, Centers for Disease Control and Prevention.
Lotze MT, Dallal RM, Kirkwood JM, Flickinger JC. Cutaneous melanoma. In DeVita VT, Rosenberg SA, Hellman S. (eds.), Principles and Practice of Oncology, 6th ed. Philadelphia: Lippincott, 2001.
Bleyer A, O’Leary M, Barr R, Ries LAG (eds): Cancer epidemiology in older adolescents and young adults 15 to 29 years of age, including SEER incidence and survival: 1975-2000. Bethesda, MD: National Cancer Institute; 2006.
SEER Cancer Stat Facts: Melanoma of the Skin. National Cancer Institute. Bethesda, MD, https://seer.cancer.gov/statfacts/html/melan.html
Siegel RL, Miller KD, Jemal A. Cancer statistics, 2019. CA Cancer J Clin. 2019; doi: 10.3322/caac.21551
Agbai ON, Buster K, Sanchez M, Hernandez C, Kundu RV, Chiu M, Roberts WE, Draelos ZD, Bhushan R, Taylor SC, Lim HW. Skin cancer and photoprotection in people of color: a review and recommendations for physicians and the public. J Am Acad Dermatol. 2014;70(4):748-62.
Wessely A, Steeb T, Erdmann M, et al. The Role of Immune Checkpoint Blockade in Uveal Melanoma. Int J Mol Sci. 2020;21(3):879. Published 2020 Jan 29. doi:10.3390/ijms21030879.
Goldemberg DC, Thuler LCS, de Melo AC. An Update on Mucosal Melanoma: Future Directions. Acta Dermatovenerol Croat. 2019;27(1):11‐15.
Lucas RM, McMichael AJ, Armstrong BK, Smith WT. Estimating the global disease burden due to ultraviolet radiation exposure. Int J Epidemiol. 2008;37(3):654-667.
Wu S, Han J, Laden F, Qureshi AA. Long-term ultraviolet flux, other potential risk factors, and skin cancer risk: a cohort study. Cancer Epidemiol Biomar Prev; 2014. 23(6); 1080-1089.
IARC Working Group. The association of use of sunbeds with cutaneous malignant melanoma and other skin cancers: a systematic review. Int J Cancer. 2006; 120: 1116-1122.
Dennis LK, Lowe JB. Does artificial UV use prior to spring break protect students from sunburns during spring break? Photodermatol Photoimmunol Photomed. 2013;29(3):140-148.
Wu S, Han J, Laden F, Qureshi AA. Long-term ultraviolet flux, other potential risk factors, and skin cancer risk: a cohort study. Cancer Epidemiol Biomar Prev; 2014. 23(6); 1080-1089.



